Intensive care units (ICUs)
What is an intensive care unit (ICU)?
Intensive care refers to the specialised treatment given to patients who are acutely unwell and require critical medical care.
An intensive care unit (ICU) provides the critical care and life support for acutely ill and injured patients.
Unless you are an emergency admission, you will need a referral from your doctor or specialist to be admitted to ICU.
Who is cared for in ICU?
Patients may have a planned admission following surgery, an unexpected admission after an accident or be admitted because of a sudden and critical deterioration to their health.
ICU teams are multi-disciplinary, made up of highly skilled intensive care nurses, doctors and specialists trained in providing critical care for patients with a variety of medical, surgical and trauma conditions.
Some hospital ICUs specialise in providing care for particular health conditions or injuries including:
- major trauma
- severe burns
- respiratory failure
- organ transplants
- complex spinal surgery
- cardiothoracic surgery.
What to expect in ICU
ICU is one of the most critically functioning operational environments in a hospital.
Every ICU in a hospital has a different environment that will reflect the specialist medical and surgical procedures they perform.
Most ICUs are fairly large sterile areas with a high concentration of specialised, technical and monitoring equipment needed to care for critically ill patients.
The ICU environment can be confronting for some patients and visitors who may find the activity, sounds, machines, tubes and monitors intimidating.
When you visit someone you care about in ICU it can be an uncomfortable experience – you may feel helpless, overwhelmed, frustrated and sad. Your feelings and apprehension are understood by the staff that provide support for the people you care about.
Typically ICU also has a higher ratio of doctors and nurses to patients.
ICU equipment
It can be a frightening and uncertain time for you, family and friends to see people you care about being monitored and supported by machines.
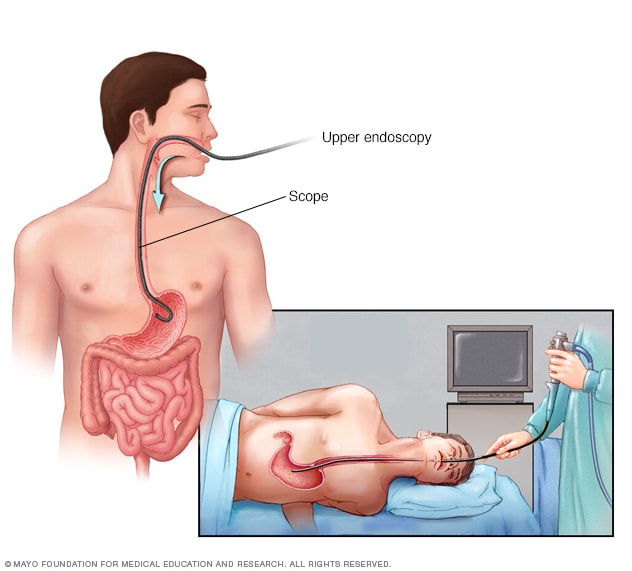
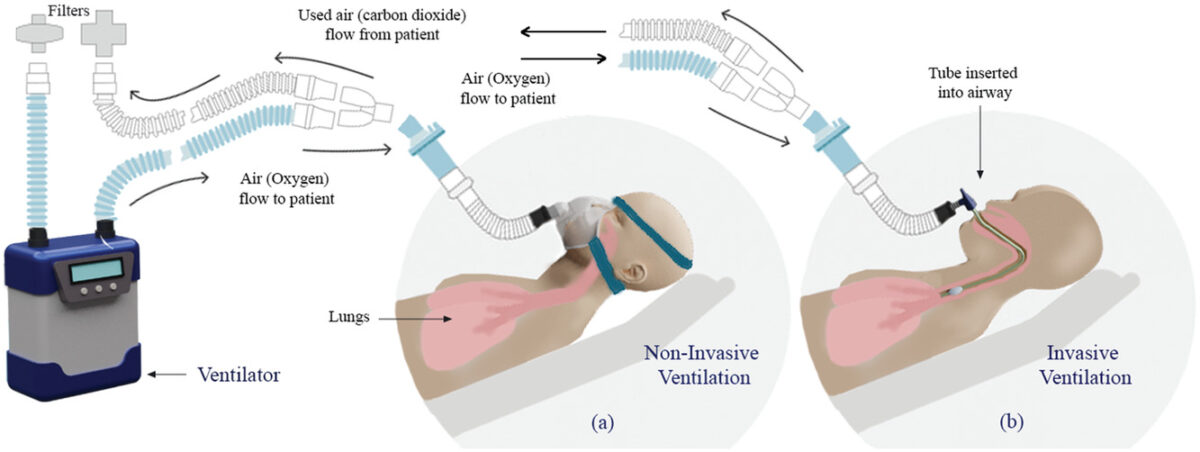
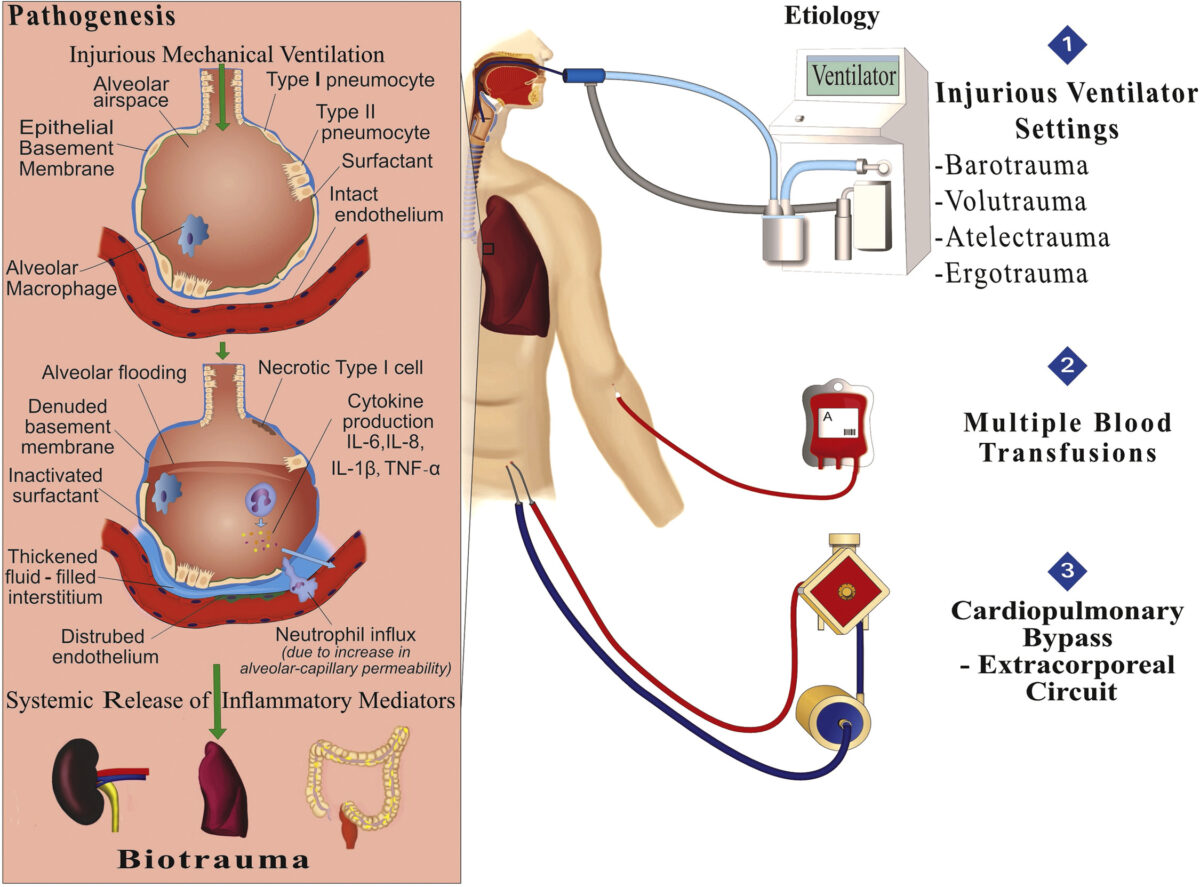
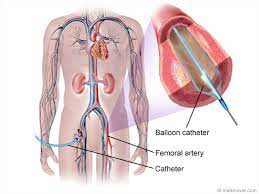
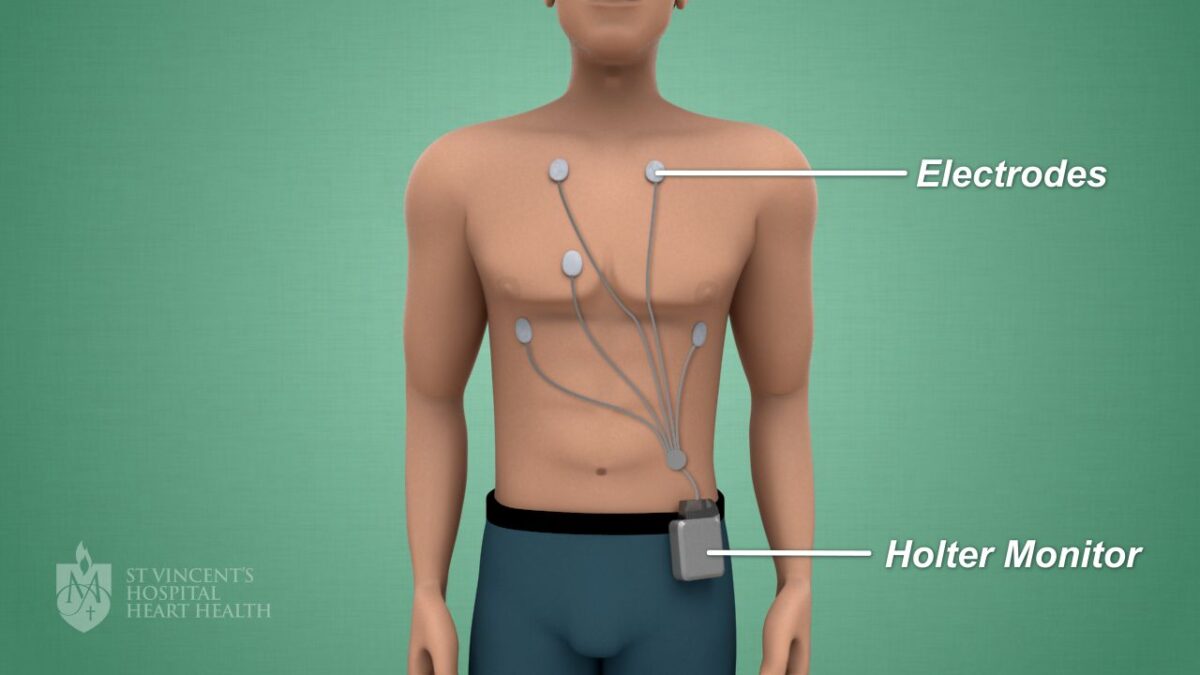
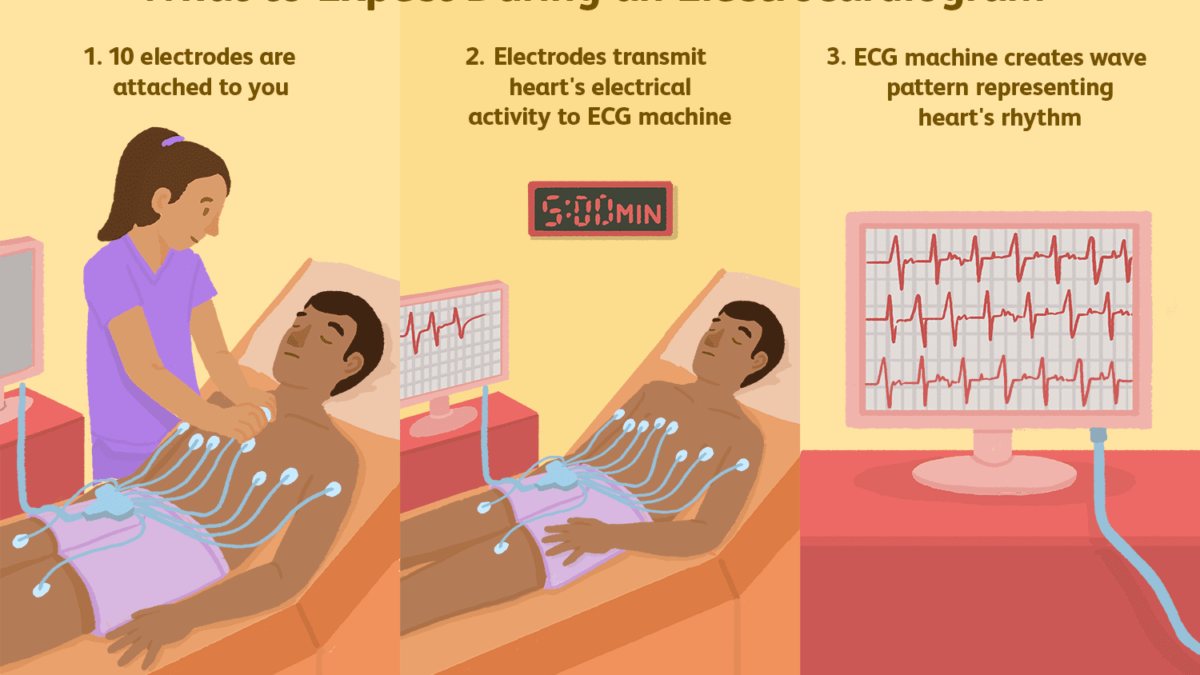
In ICU you will see many patients connected to a heart monitor, others will be supported with breathing assistance from artificial ventilators, be on dialysis machines and receiving a variety of intravenous infusions via tubes and drips.
Be prepared to see lots of lines, tubes, wires and monitoring equipment. Almost all ICU equipment uses alarms to let staff know about a change in a patient’s condition. Not all equipment alarms signal an emergency situation.
Visitors
Every ICU has a visitor policy to ensure the wellbeing of their patients. You will need to ask ICU hospital staff about their specific visiting hours and requirements.
Visiting is usually restricted to people the patient considers to be immediate family.
If you are feeling unwell or have an existing health condition you should reconsider visiting ICU or discuss your circumstances with ICU staff before you plan to visit.
Hygiene
As intensive care patients are very vulnerable to infections, it is important that visitors wash their hands before entering ICU to prevent transferring infection.
Mobile phones
Mobile phones should be turned off in ICU as they may interfere with vital electrical equipment supporting patients.
Gifts
Restrictions are in place to allow easy access to vital medical equipment and to patients.
If you are unsure what you can bring with you check with ICU staff before you plan to visit.
Patient and family support services
Counselling
Admission to ICU because of critical illness or accident can have a huge physical and emotional impact on your life and your family.
Some ICUs have a dedicated counsellor to provide support for patients and their families. These counsellors are highly experienced and have a thorough knowledge of ICU procedures.
Hospital counselling support services are also available at all major hospitals.
Pastoral care
For many people, emotional and spiritual thoughts tend to surface when someone they care about is in a critical condition in hospital.
Many hospitals provide chaplaincy and pastoral counselling services for patients, families and staff who need compassionate, professional and spiritual guidance and support.
Some hospitals also have a non-denominational chapel available for times of reflection and prayer.
Interpreter service
An interpreter service is available for patients and families if English is not your first language.
These interpreters are specifically trained to interpret medical terms into other languages. It is important that you use this service if you are having problems understanding doctors explaining information or are being asked to provide consent for medical procedures.
Speak to ICU staff if you would like to use interpreting services.